Glaucoma as Neurologic Disorder Rather Than Eye Disease?
ScienceDaily (Mar. 7, 2012) - A new paradigm to explain Glaucoma is rapidly emerging, and it is generating brain-based treatment advances that may ultimately vanquish the disease known as the "sneak thief of sight." A review now available in Ophthalmology, the journal of the American Academy of Ophthalmology, reports that some top researchers no longer think of Glaucoma solely as an eye disease. Instead, they view it as a neurologic disorder that causes nerve cells in the brain to degenerate and die, similar to what occurs in Parkinson disease and in Alzheimer's. The review, led by Jeffrey L Goldberg, M.D., Ph.D., assistant professor of ophthalmology at the Bascom Palmer Eye Institute and Interdisciplinary Stem Cell Institute, describes treatment advances that are either being tested in patients or are scheduled to begin clinical trials soon.
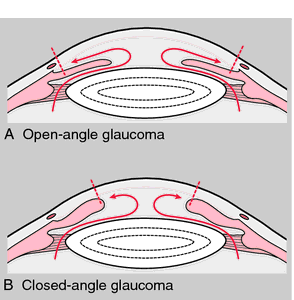
Glaucoma is the most common cause of irreversible blindness worldwide. For many years, the prevailing theory was that vision damage in Glaucoma patients was caused by abnormally high pressure inside the eye, known as intraocular pressure (IOP). As a result, lowering IOP was the only goal of those who developed surgical techniques and medications to treat Glaucoma. Creating tests and instruments to measure and track IOP was crucial to that effort. Today, a patient's IOP is no longer the only measurement an ophthalmologist uses to diagnose Glaucoma, although it is still a key part of deciding how to care for the patient. IOP-lowering medications and surgical techniques continue to be effective ways to protect Glaucoma patients' eyes and vision. Tracking changes in IOP over time informs the doctor whether the treatment plan is working.
But even when surgery or medication successfully lowers IOP, vision loss continues in some Glaucoma patients. Also, some patients find it difficult to use eye drop medications as prescribed by their physicians. These significant shortcomings spurred researchers to look beyond IOP as a cause of Glaucoma and focus of treatment.
The new research paradigm focuses on the damage that occurs in a type of nerve cell called retinal ganglion cells (RGCs), which are vital to the ability to see. These cells connect the eye to the brain through the optic nerve.
RGC-targeted Glaucoma treatments now in clinical trials include: medications injected into the eye that deliver survival and growth factors to RGCs; medications known to be useful for stroke and Alzheimer's, such as cytidine-5-diphosphocholine; and electrical stimulation of RGCs, delivered via tiny electrodes implanted in contact lenses or other external devices. Human trials of stem cell therapies are in the planning stages.
"As researchers turn their attention to the mechanisms that cause retinal ganglion cells to degenerate and die, they are discovering ways to protect, enhance and even regenerate these vital cells," said Dr. Goldberg. "Understanding how to prevent damage and improve healthy function in these neurons may ultimately lead to sight-saving treatments for Glaucoma and other degenerative eye diseases."
If this neurologically-based research succeeds, future Glaucoma treatments may not only prevent Glaucoma from stealing patients' eyesight, but may actually restore vision. Scientists also hope that their in-depth exploration of RGCs will help them determine what factors, such as genetics, make some people more vulnerable to Glaucoma.
http://www.sciencedaily.com/releases/2012/03/120307094659.htm
Story Source:
The above story is reprinted from materials provided by American Academy of Ophthalmology.
Note: Materials may be edited for content and length. For further information, please contact the source cited above.










No comments:
Post a Comment